Headline News
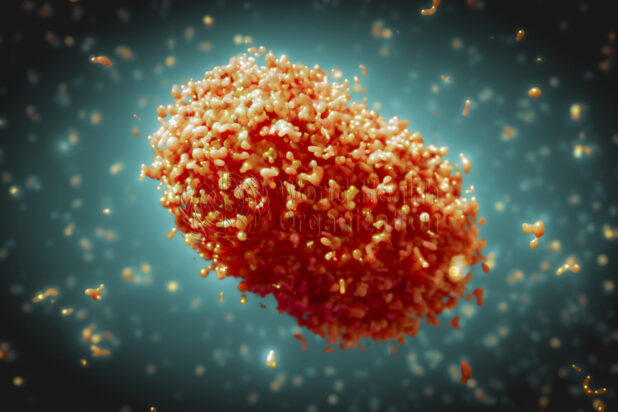
Monkeypox virus: what to know about it
June 21, 2022
By Mike Riley
Local Journalism Initiative Reporter
Monkeypox is a viral zoonotic infectious disease, meaning that it’s transmitting from animals to humans. It is found in parts of central and west Africa and infections usually occur with exposure to infected animals or contaminated materials. This is the first time that cases have been reported in Canada, although limited cases have been seen before in the U.K., the U.S., Israel and Singapore. Hastings Prince Edward Health Unit’s medical officer of health Dr. Ethan Toumishey provides an update about the Monkeypox virus and what’s happening with it here in Canada.
Dr. Toumishey told Bancroft this Week on June 9 that while Monkeypox is something that’s been hitting the news now, it’s a known quantity from a global health perspective and has been for some time.
“So, we have a good idea on the virus and its characteristics. There is a knowledge of vaccines and how that would work as well as treatments that would be available. So, for that clinical knowledge, that is absolutely there and helps us to prepare,” he says.
According to an HPEPH June 2 update, Dr. Toumishey said that basic health measures that everyone should be practicing at all times will help to prevent the spread of Monkeypox. These measures include; staying home if you’re sick or have skin sores, engaging in respiratory etiquette (wearing a mask, covering your coughs and sneezes), practicing good hand hygiene and practicing safer sex. Additionally, avoiding close physical contact, including sexual contact, with an individual who may have or does have Monkeypox is highly recommended.
Toumishey says that compared to COVID-19, Monkeypox is much less transmissible, and is spread through prolonged close contact with those who have the virus and have symptoms. Symptoms usually develop five to 21 days after being exposed and they occur in stages that last from two to four weeks. Somebody with Monkeypox can be contagious and spread the virus from one to five days before the rash develops and continues to be contagious until the scabs have fallen off and their skin has healed.
The first stage symptoms of Monkeypox are; fever, chills, swollen lymph nodes, headache, muscle pain, joint pain, back pain and exhaustion. Within a few days of these symptoms, a rash develops, usually on the face first and then it spreads to the rest of the body. According to the HPEPH, this rash, which can last for two to four weeks, can affect the mucous membranes in the mouth, tongue and genitalia, and can also be evident on the palms of hands and the soles of the sufferers’ feet. The rash progresses through the following stages; macules, papules, vesicles, pustules and scabs.
Toumishey emphasizes that Monkeypox doesn’t typically result in as many cases or spread as quickly, so there are relatively low case numbers in Ontario and so far, none in Hastings Prince Edward.
“We are very committed with the province and with our health care providers so people are informed on what to do and encourage people that if they know they’ve been exposed to a case or worried that they may be or having symptoms that they’re connecting with their healthcare provider,” he says.
Most at risk from the Monkeypox virus, according to Toumishey are those who are immunocompromised, those who may come into contact with infected wild animals (especially in parts of Africa where it’s endemic) and materials that have been contaminated and those who do not have ready access to healthcare options that would protect them from the virus.
“It can be a very serious illness. Now there are different strains of Monkeypox. The cases we’re seeing in Canada, the U.S. and Europe are of the milder strain, so that’s a positive. Very rarely, especially when people are lacking access to appropriate medical care that this can be a very serious infection and it can be life threatening. The caveat I would say is that in the presence of being able to access appropriate medical care that would be very rare. So, it’s important that if people are feeling like they’ve been exposed or have symptoms the crucial step is going to seek medical attention and connecting with your healthcare provider. That would be the biggest step,” he says.
Regarding whether there have been any changes to the Monkeypox virus that would see it perhaps becoming more virulent, Toumishey says that it hasn’t been noted at this time.
“There doesn’t seem to have been a particular change so far with the virus that’s making it more infectious or changing how it’s behaving in a big way. But that’s being very carefully examined from the international scientific community. They’re keeping a very close eye on the virus sequences and if anything looks to be changing, then that would be communicated if we’re seeing anything change that way,” he says.
Toumishey says that there are vaccines that are effective at treating Monkeypox, but typically with the numbers seen thus far, they’re used to treat the outbreak areas versus a broad population vaccination like we’ve seen with COVID-19.
“When we look at the overall population risk from Monkeypox, it would be very low. There is a lot of work that’s going into the investigation of these clusters and outbreaks but we have all the tools available that we should be able to get some progress on this.”
Subsequent to Bancroft This Week speaking with Dr. Toumishey, the World Health Organization director general Tedros Adhanom Ghebreyesus announced he’d be convening an emergency committee on June 23 because the virus had shown “unusual” recent behaviour by spreading beyond parts of Africa where it’s endemic.
As of June 14, more than 1,600 cases and nearly 1,500 suspected cases had been reported in 39 countries this year. In Canada as of June 17, the Public Health Agency of Canada said there were 168 cases in the country; 141 cases in Quebec, 21 in Ontario, four in Alberta and two in British Columbia. However, an Ipsos poll conducted for Global News on June 17 found that 67 per cent of Canadians weren’t worried and felt that public health officials would be able to contain the spread of the Monkeypox virus.
The WHO also released its interim guidance on vaccines and immunization from Monkeypox on June 14. According to the overview on the WHO website, the goal of the global outbreak response for Monkeypox is “to control the outbreak and effectively use strong public health measures to prevent further spread through judicious use of vaccines.”
The interim guidance was developed with the advice and support of the Strategic Advisory Group of Experts Ad hoc working group on smallpox and monkeypox vaccines. Their interim recommendations are as follows; mass vaccination if not required or recommended at this time, post exposure preventative vaccine recommended for contacts of cases within four days to prevent onset of disease, pre-exposure preventative vaccination recommended for health care workers at risk, laboratory personnel, clinical laboratory staff and others at risk, vaccination programs must be backed by thorough surveillance and contact tracing, a strong information campaign and a robust pharmacovigilance, which is the pharmaceutical science relating to the collection, detection, assessment, monitoring and prevention of adverse affects with pharmaceutical products, in this case, the smallpox or monkeypox vaccines. The WHO says that further guidance will be issued as more information comes to light.

















